Scientists and researchers have been working tirelessly to develop rapid, accurate diagnostics, life-saving vaccines and various treatments for COVID-19. To help clinicians triage patients and monitor patients’ responses to therapies, developing prognostic biomarkers is also important. A key part of this vital work is understanding how the immune system responds to the SARS-CoV-2 virus (which causes COVID-19) and which immune cell types play a critical role in fighting the virus.
Flow cytometry is a highly important technology in the study of immune cells and their responses. As a pioneer and global leader in the flow cytometry field, BD, along with Science magazine and the FlowTex consortium, hosted a webinar: “Monitoring the Immune System to Fight COVID-19: CD4 Status, Lymphopenia* and Infectivity.” The event drew thousands, as highly respected experts, well known for applying flow cytometry in the study of the immune system and infectious diseases, shared their latest findings and innovations in the biomarker space for COVID-19.
Understanding the role of T cells in COVID-19
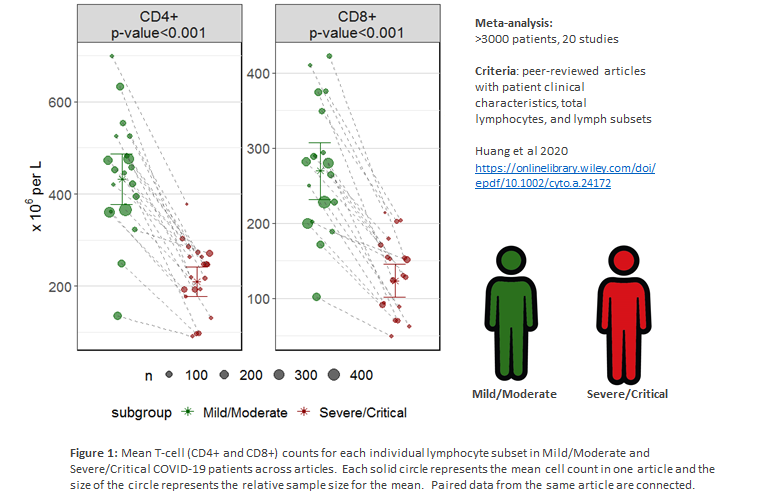
In the case of COVID-19, two types of lymphocytes–CD4 and CD8 T cells–have generated the most attention. This interest is based on emerging research showing that the CD4+ and CD8+ T cell response to SARS-CoV-2 influences whether a patient will progress to severe disease, and this connection may be used to predict clinical outcomes1.
Maurice O’Gorman, PhD, MSc, chief of laboratory medicine and director of the Diagnostic Immunology and Flow Cytometry Laboratory at Children’s Hospital Los Angeles, provided an overview of the COVID-19 diagnostic guidelines used in China and recent literature showing a correlation between low cell counts (loss) of immune cells, particularly CD4+ and CD8+ T cells, and COVID-19 disease severity2. CD4+ T cell loss is especially important as this cell type is known to mediate the generation of antibodies (and immunity) against the virus.
Dr. O’Gorman has since published a meta-analysis demonstrating the potential of CD4+ and CD8+ T cell counts to serve as prognostic biomarkers for predicting disease severity in COVID-19 patients (Figure 1)3.
Cytokine storm in COVID-19 patients
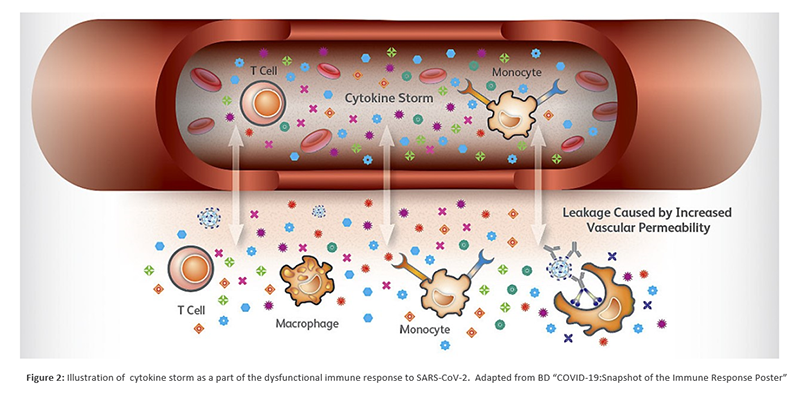
Andrea Cossarizza, MD, PhD, vice dean of the School of Medicine at the University of Modena and Reggio Emilia in Italy, shared insights on how monitoring the immune system was helping aid in the fight against COVID-19. Dr. Cossarizza discussed how specific immune cells respond to SARS-CoV-2 and skew the immune response in an unproductive way, leading to ineffective control of the virus, and in some cases, causing harm to the patient due to an overactive and dysfunctional immune response (Figure 2) that creates excessive inflammation (i.e., a cytokine storm)4.
He also presented data on another cytokine, IL-17, a pro-inflammatory protein that is part of the immune system. This cytokine was shown to be upregulated in COVID-19 patients. Dr. Cossarizza hypothesized that, like IL-6, IL-17 could be blocked using drugs that are already available and used in other disease.
Positive steps toward therapies and disease monitoring
These insights can help unlock the mysteries of the virus infection process and will help the research community develop life-saving therapeutics and vaccines, and also identify biomarkers that will help the medical community determine the patients who are at greatest risk for developing severe disease.
We thank these outstanding experts for taking the time to share their research findings and helping inform the scientific and medical community, along with individuals around the world, better understand this important area of research.
*A condition where there is a lower than normal number of lymphocytes, a type of white blood cell.
Visit bd.com/COVID-19 for additional information on how BD is addressing the Coronavirus.
Watch the Monitoring the immune system to fight COVID-19: CD4 status, lymphopenia, and infectivity webinar replay.
- Tay MZ, Poh CM, Rénia L, et al. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol (2020);20: 363–374. doi: 10.1038/s41577-020-0311-8
- Jin Y, Cai L, Cheng Z, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Military Med Res (2020); 7:4. doi: 10.1186/s40779-020-0233-6
- Huang W, Berube J, McNamara M, et al. Lymphocyte Subset Counts in COVID-19 Patients: A Meta-Analysis. Cytometry. Part A: the Journal of the International Society for Analytical Cytology. 2020 Jun; doi: 10.1002/cytoa.24172
- Cossarizza A, De Biasi S, Guaraldi G, Girardis M, Mussini C, & Modena Covid-19 Working Group (MoCo19)# (2020). SARS-CoV-2, the Virus that Causes COVID-19: Cytometry and the New Challenge for Global Health. Cytometry. Part A: the journal of the International Society for Analytical Cytology 2020; 97(4): 340–343. doi: 10.1002/cyto.a.24002
BD and the BD Logo are trademarks of Becton, Dickinson and Company. All other trademarks are the property of their respective owners. © 2020 BD. All rights reserved
Subscribe to receive BD blog alerts