
Sepsis, severe sepsis and renal insufficiency/failure rate as top three conditions associated with COVID-19 hospital mortality complications
By Kalvin Yu, MD, FIDSA, Vice President of U.S. Medical Affairs and Vikas Gupta, Pharm.D., Director of Medical Affairs
As the world becomes an interdependent information sharing community in parallel with an increasingly global economy, emerging infectious diseases have been occurring with greater frequency during the past few decades. None have tested the U.S. health care system’s capacity or resiliency like COVID-19 – forever changing the way that we think about future outbreaks and how we manage the related unintended consequences. As we pass the two-year mark of the COVID-19 pandemic, we’re launching BD Infectious Disease Insights to dig deeper into today’s most prominent infectious disease trends.
BD Infectious Disease Insights will leverage the depth and breadth of our data to serve as an ongoing bellwether on the state of infectious diseases in the U.S., backed by clinical insights on how to increase awareness, preparedness and endurance. This marks our inaugural blog in the BD Infectious Disease Insights series and examines key trends in disease severity and health care utilization during the Omicron wave.
Throughout the COVID-19 pandemic, we’ve closely analyzed how the U.S. health care system was faring against COVID-19 through our timely network of U.S. clinical data (i.e., laboratory results, pharmacy orders, and outcomes data). Our aggregate level data from more than 250 U.S. facilities is shared with the Centers for Disease Control and Prevention (CDC) weekly (displayed biweekly on the public website) and provides us with the opportunity to identify near real-time patient severity indicators. More importantly, it helps us examine how to handle the current caseload and the adverse collateral burden it will place on our health care system.
Several indicators show we’re reaching a much-needed reprieve in disease severity this Spring. We’ve seen that Omicron is largely more contagious, but less severe in the vaccinated, than previous variants. By now, that is no surprise, but it is worth digging into just how rapidly the severity trend line has decreased. For example, the hospital mortality rate lowered by approximately 53% in just over 100 days. The late November peak reached 14.1% -- and the most recent week (March 19) was at 6.6%.
The data also show that:
- During the pandemic, the overall hospital mortality for COVID-19 positive patients with sepsis, severe sepsis, renal insufficiency or failure is approximately 2.5 times greater as compared to all COVID-19 positive admissions (24.9% vs. 10.3%). The weekly hospital mortality rate in patients with sepsis, severe sepsis, renal insufficiency or failure is at 14.5% for March 19, 2022 -- down from 35.5% in late November 2021 (see Figure 1).
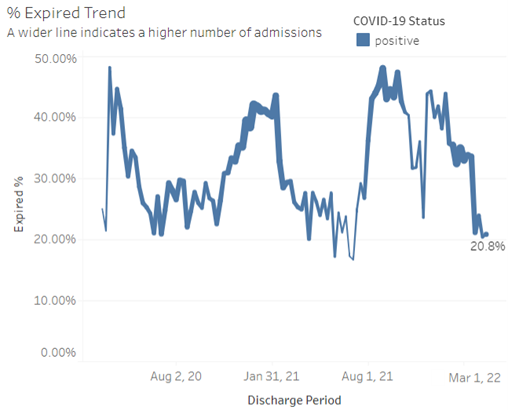
- The weekly hospital mortality rate for patients admitted to the intensive care unit has dropped to 20.8% as of March 19, 2022 -- down from 44.3% in late November 2021 (see Figure 2).
Figure 1. Mortality trends in admissions for patients with sepsis, severe sepsis, and renal insufficiency or failure (weekly discharges through March 19, 2022)
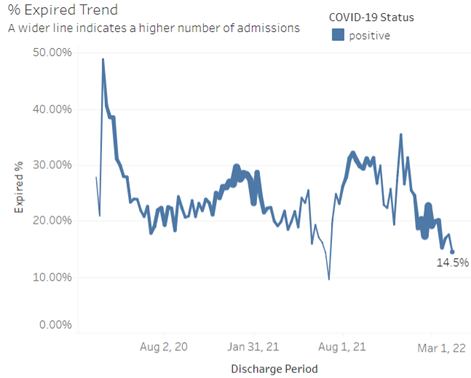
Figure 2. Mortality trends for patients admitted to the ICU (discharges through March 19, 2022)
We recognize that these numbers naturally cause speculation that we’re approaching a period where COVID-19 is clinically considered a milder disease, and ultimately potentially reaching the endemic phase. However, the evolutionary path of COVID-19 remains unclear and careful monitoring is critical.
Managing COVID-19 effectively will require more than solely tracking case numbers. We’ve reached a moment in time where we are seeing increasing levels of population immunity through a combination of infection and vaccinations as well as a more immune-evasive but less virulent virus – leading many officials to roll back mitigation efforts like masking, testing and avoiding gathering. The CDC has also updated guidance to measure community risk for COVID-19 by three primary metrics: new hospitalizations for COVID-19, current hospital beds occupied by COVID-19 patients and new COVID-19 cases.
These new metrics further underscore the importance of leveraging in-depth data to measure a broader view of near-term risk beyond case numbers (i.e., case severity and pending hospitalizations). Our data provide a timely and early signal of the severity of outbreaks and can ultimately guide mitigation efforts both nationally and locally. Even now, a Delta-Omicron hybrid variant has emerged in Europe and the U.S., serving as a reminder that vigilant surveillance and related hospital and mortality trends will be critical to health care delivery and supply chain planning moving forward.
The role of infectious disease monitoring will remain paramount for hospitals, governments, and society at large. We’re committed to keeping our focus on the most important trends in infectious diseases, and hope that you’ll follow the conversation here. To subscribe to this series: visit https://news.bd.com/blog.
Subscribe to receive BD blog alerts