Recent data show that inadequate antimicrobial treatment is more common among COVID-19 positive patients – leading to prolonged hospital stays.
By Kalvin Yu, MD, FIDSA, Vice President of U.S. Medical Affairs and Vikas Gupta, Pharm.D., Director of Medical Affairs
Antimicrobial resistance (AMR) is the ability of microorganisms (such as bacteria, fungi, viruses, or protozoa) to nullify the effects of antimicrobial drugs, resulting in these drugs becoming ineffective. Seasonally, we often see that bacterial AMR surges during peaks in cold and flu activity. During this period, it’s common for patients to receive higher and unnecessary antimicrobial treatment in both the inpatient and outpatient setting.
We have previously shown that hospitalized patients prescribed inadequate empiric therapy leads to worse outcomes, prolonged hospital stays and, in some cases, mortalities. Factors that often contribute to inadequate antimicrobial treatment among hospitalized patients include prior antibiotic use, a multiple day hospital stay or ongoing mechanical ventilation.
Health care systems face a future of not only managing routine respiratory virus illnesses (like RSV, metapneumovirus, other cold viruses and the flu), but also the new “x-factor” of continued COVID-19 surges. To understand the extent that AMR may further impact this challenge, we analyzed hospital admissions in our database of approximately 250 U.S. health care facilities to compare how inadequate antimicrobial treatment varied before and during the COVID-19 pandemic.
Overall, inadequate antimicrobial treatment rates were highest among COVID-19 positive patients. Approximately one in four (25.9 percent) of COVID-19 positive patients received inadequate treatment between March 2020 and October 2021. During that same period, 20.3 percent of patients who tested negative for SARS-CoV-2 also received inadequate therapy – which was consistent with pre-pandemic rates (20.2 percent).
Additional findings include:
- Inadequate antimicrobial treatment leads to longer hospital stays among COVID-19 positive patients. On average, COVID-19 positive patients that received inadequate therapy stayed in the hospital 1.5 days longer than those that received adequate therapy (18.7 days vs. 17.2 days) – while those who tested negative experienced an average hospital stay of 13.9 days.
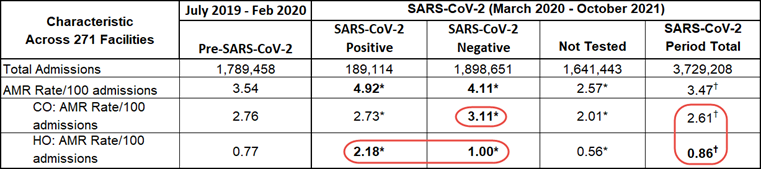
- For hospital onset pathogens, AMR rates were significantly higher overall in the pandemic period – particularly for patients who tested positive for COVID-19. (See Table 1.)
TABLE 1
We presented these finding at this week’s World Vaccine Congress Washington – the largest and longest-running conference dedicated to vaccine advocacy and research – to underscore the important role that vaccinations can play in mitigating the unintended consequences of flu and COVID-19 infections, particularly hospitalizations that ultimately contribute to the spread of AMR pathogens and associated inadequate treatment. Targeted vaccination in high-risk demographics may be our most immediately viable defense in keeping vulnerable populations healthy or less severely ill.
As health systems continue to monitor capacity, more resources and staffing are needed to support vaccine and antimicrobial stewardship programs. At BD, we support health systems through capabilities that aim to identify the most appropriate and timely use of antimicrobials with the goal of containing and reducing AMR. These capabilities are more important than ever – particularly as health systems manage seasonal health care needs in tandem with COVID-19.
Our capabilities include:
- Supporting infection control guidelines through products and services designed to help clinicians improve patient outcomes through the standardization of care.
- Expanding diagnostic testing to classify infections and guide therapies – helping clinicians to implement effective antimicrobial stewardship interventions.
- Advancing medication management through a connected medication management system with technologies, analytics, and surveillance tools to ensure the appropriate utilization of medications.
About BD Infectious Disease Insights
Emerging infectious diseases have been increasing in frequency during the past few decades. None have tested the U.S. health care system’s capacity or resiliency like COVID-19 – forever changing the way that we think about future outbreaks and how we manage the related unintended consequences. The BD Infectious Disease Insights series investigates today’s most prominent infectious disease trends. The series will leverage the depth and breadth of our data to serve as an ongoing bellwether on the state of infectious diseases in the U.S., backed by clinical insights on how to increase overall awareness and preparedness.
To subscribe to this series: visit https://news.bd.com/blog.
Subscribe to receive BD blog alerts